

Positive outcomes in the elderly include reduced falls, improved quality of life and mortality. ĭeprescribing was studied in earlier trials without causing significant adverse effects Interventions may be initiated by either physician, pharmacist or the entire multidisciplinary team, using either a general or specific deprescribing algorithm (e.g. Inappropriate drug use and side effects were identified in these patients. Similarly, in another local study, patients in 3 nursing homes were on an average of 5.32 medications. In Singapore, statistics from a public hospital found that more than half of all patients were discharged with at least five chronic medications. ĭeprescribing is more critical in the elderly due to the higher prevalence of polypharmacy and inappropriate medication use. Finally, the routine supplementation of multivitamins and vitamin B complex remains controversial, beyond the replacement of individual components for established medical conditions (e.g. glucosamine, chondroitin) have not demonstrated significant benefits in recent trials for the management of osteoarthritis and are potential targets for deprescribing. analgesics, laxatives) are commonly prescribed long term without clear indications. Amongst the latter, symptomatic medicine (e.g. We chose American Geriatric Society’s Beer’s List of Potentially Inappropriate Medicine (a common guide for geriatric deprescribing) and some locally important medicine. These include ascertaining the patient’s current medication and their indications, considering their individual risk of harm, assessing each medication’s current or future benefit, harm or burden, prioritising them for discontinuation and implementing a discontinuation regimen with close monitoring for benefits and harm.

Five distinct steps of deprescribing had been described by Scott. Multidisciplinary interventions are generally more effective than monodisciplinary interventions in reducing inappropriate medicines. ĭeprescribing has to be patient-centric with shared decisions between patients, caregivers and the healthcare team. It should be perceived as part of the treatment continuum, where medications are initiated, dose-adjusted, discontinued, added or substituted, to optimise the quality of life and life expectancy.
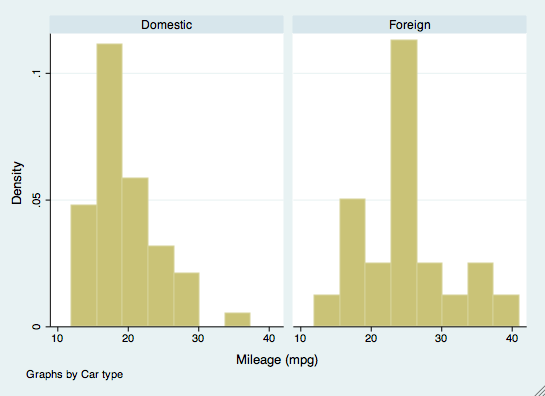
STATA MEDIAN PROFESSIONAL
ĭeprescribing is the process of withdrawal of an inappropriate medication, supervised by a healthcare professional with the goal of managing polypharmacy and improving outcomes. This study is first registered at (protocol number: NCT03713112) on and the protocol can be accessed on. Conclusionĭeprescribing rounds can safely reduce TDD of medicine upon discharge compared to usual care in a Singaporean rehabilitation hospital.
The median rounding time was 7.09 min per patient and challenges include the inconvenience in assembling the multidisciplinary team. The intervention arm ( n = 126) experienced a greater reduction of TDD on discharge, more constipation (OR: 3.75, 95% CI:1.75–8.06, p < 0.001) and laxative re-prescriptions (OR: 2.82, 95% CI:1.30–6.12, p = 0.009) though death and hospitalisation rates were similar. Baseline characteristics were largely similar in both groups. ResultsĢ60 patients were randomised and 253 were analysed after excluding dropouts (female: 57.3% median age: 76 years). Efficacy outcomes were analysed using intention-to-treat while other outcomes were analysed as per protocol. The primary outcome is the percentage change in total daily dose (TDD) from baseline upon discharge, while the secondary outcomes are the total number of medicine, total daily cost and TDD up to day 28 postdischarge, overall side-effect rates, rounding time and the challenges. The intervention consisted of weekly multidisciplinary team-led deprescribing rounds (using five steps of deprescribing) and usual care. They were randomised using a computer generated sequence.
STATA MEDIAN TRIAL
MethodsĪn open label randomised controlled trial was conducted on patients of 65 years and above, under rehabilitation or subacute care and with prespecified medications from a Singapore rehabilitation hospital. However, the impact of deprescribing rounds remain unclear in Asian settings. Deprescribing is effective and safe in reducing polypharmacy among the elderly.


 0 kommentar(er)
0 kommentar(er)
